What Is Breast Cancer?
Breast cancer is a kind of cancer that develops from breast cells. Breast cancer usually starts off in the inner lining of milk ducts or the lobules that supply them with milk. A malignant tumor can spread to other parts of the body. A breast cancer that started off in the lobules is known as lobular carcinoma, while one that developed from the ducts is called ductal carcinoma.
Breast cancer is the most common invasive cancer in females worldwide. It accounts for 16% of all female cancers and 22.9% of invasive cancers in women. 18.2% of all cancer deaths worldwide, including both males and females, are from breast cancer.
Breast cancer rates are much higher in developed nations compared to developing ones. There are several reasons for this, with possibly life-expectancy being one of the key factors – breast cancer is more common in elderly women; women in the richest countries live much longer than those in the poorest nations. The different lifestyles and eating habits of females in rich and poor countries are also contributory factors, experts believe.
According to the National Cancer Institute, 232,340 female breast cancers and 2,240 male breast cancers are reported in the USA each year, as well as about 39,620 deaths caused by the disease.
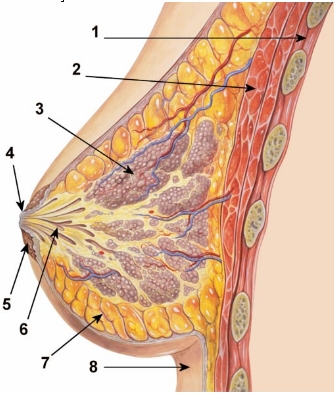
 1. Chest wall. 2. Pectoralis muscles. 3. Lobules (glands that make milk). 4. Nipple surface. 5. Areola. 6. Lactiferous duct tube that carries milk to the nipple. 7. Fatty tissue. 8. Skin.
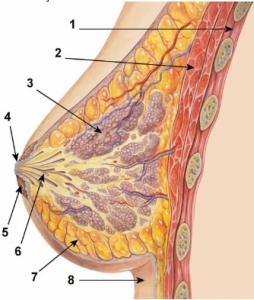
1. Chest wall. 2. Pectoralis muscles. 3. Lobules (glands that make milk). 4. Nipple surface. 5. Areola. 6. Lactiferous duct tube that carries milk to the nipple. 7. Fatty tissue. 8. Skin.
A mature human female’s breast consists of fat, connective tissue and thousands of lobules – tiny glands which produce milk. The milk of a breastfeeding mother goes through tiny ducts (tubes) and is delivered through the nipple.
The breast, like any other part of the body, consists of billions of microscopic cells. These cells multiply in an orderly fashion – new cells are made to replace the ones that died. In cancer, the cells multiply uncontrollably, and there are too many cells, progressively more and more than there should be.
Cancer that begins in the lactiferous duct (milk duct), known as ductal carcinoma, is the most common type. Cancer that begins in the lobules, known as lobular carcinoma, is much less
common.
What is the difference between invasive and non-invasive breast cancer?
Invasive breast cancer – the cancer cells break out from inside the lobules or ducts and invade nearby tissue. With this type of cancer, the abnormal cells can reach the lymph nodes, and eventually make their way to other organs (metastasis), such as the bones, liver or lungs. The abnormal (cancer) cells can travel through the bloodstream or the lymphatic system to other parts of the body; either early on in the disease, or later.
Non-invasive breast cancer – this is when the cancer is still inside its place of origin and has not broken out. Lobular carcinoma in situ is when the cancer is still inside the lobules, while ductal carcinoma in situ is when they are still inside the milk ducts. “In situ” means “in its original place”. Sometimes, this type of breast cancer is called “pre-cancerous”; this means that although the abnormal cells have not spread outside their place of origin, they can eventually develop into invasive breast cancer.
What are the signs and symptoms of breast cancer?
A symptom is only felt by the patient, and is described to the doctor or nurse, such as a headache or pain. A sign is something the patient and others can detect, for example, a rash or swelling.
The first symptoms of breast cancer are usually an area of thickened tissue in the woman’s breast, or a lump. The majority of lumps are not cancerous; however, women should get them checked by a health care professional.
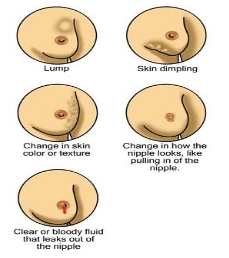
Women who detect any of the following signs or symptoms should tell their doctor:
- A lump in a breast
- A pain in the armpits or breast that does not seem to be related to the woman’s menstrual period
- Pitting or redness of the skin of the breast; like the skin of an orange
- A rash around (or on) one of the nipples
- A swelling (lump) in one of the armpits
- An area of thickened tissue in a breast
- One of the nipples has a discharge; sometimes it may contain blood
- The nipple changes in appearance; it may become sunken or inverted
- The size or the shape of the breast changes
- The nipple-skin or breast-skin may have started to peel, scale or flake
What are the causes of breast cancer?
Experts are not sure what causes breast cancer. It is hard to say why one person develops the disease while another does not. We know that some risk factors can impact on a woman’s likelihood of developing breast cancer.
- Getting older – the older a woman gets, the higher is her risk of developing breast cancer; age is a risk factor. Over 80% of all female breast cancers occur among women aged 50+ years (after the menopause).
- Genetics – women who have a close relative who has/had breast or ovarian cancer are more likely to develop breast cancer. If two close family members develop the disease, it does not necessarily mean they shared the genes that make them more vulnerable, because breast cancer is a relatively common cancer.The majority of breast cancers are not hereditary.
Women who carry the BRCA1 and BRCA2 genes have a considerably higher risk of developing breast and/or ovarian cancer. These genes can be inherited. TP53, another gene, is also linked to greater breast cancer risk.
- A history of breast cancer – women who have had breast cancer, even non-invasive cancer, are more likely to develop the disease again, compared to women who have no history of the disease.
- Having had certain types of breast lumps – women who have had some types of benign (non-cancerous) breast lumps are more likely to develop cancer later on. Examples include atypical ductal hyperplasia or lobular carcinoma in situ.
- Dense breast tissue – women with more dense breast tissue have a greater chance of developing breast cancer.
- Estrogen exposure – women who started having periods earlier or entered menopause later than usual have a higher risk of developing breast cancer. This is because their bodies have been exposed to estrogen for longer. Estrogen exposure begins when periods start, and drops dramatically during the menopause.
- Obesity – post-menopausal obese and overweight women may have a higher risk of developing breast cancer. Experts say that there are higher levels of estrogen in obese menopausal women, which may be the cause of the higher risk.
- Height – taller-than-average women have a slightly greater likelihood of developing breast cancer than shorter-than-average women. Experts are not sure why.
- Alcohol consumption – the more alcohol a woman regularly drinks, the higher her risk of developing breast cancer is. Experts say that if a woman wants to drink, she should not exceed one alcoholic beverage per day.
- Radiation exposure – undergoing X-rays and CT scans may raise a woman’s risk of developing breast cancer slightly.
- HRT (hormone replacement therapy) – both forms, combined and estrogen-only HRT therapies may increase a woman’s risk of developing breast cancer slightly. Combined HRT causes a higher risk.
- Certain jobs – French researchers found that women who worked at night prior to a first pregnancy had a higher risk of eventually developing breast cancer.
Canadian researchers found that certain jobs, especially those that bring the human body into contact with possible carcinogens and endocrine disruptors are linked to a higher risk of developing breast cancer. Examples include bar/gambling, automotive plastics manufacturing, metal-working, food canning and agriculture. They reported their findings in the November 2012 issue of Environmental Health.
- Cosmetic implants may undermine breast cancer survival – women who have cosmetic breast implants and develop breast cancer may have a higher risk of dying prematurely form the disease compared to other females, researchers from Canada.
Diagnosing breast cancer
Women are usually diagnosed with breast cancer after a routine breast cancer screening, or after detecting certain signs and symptoms and seeing their doctor about them.
If a woman detects any of the breast cancer signs and symptoms described above, she should speak to her doctor immediately. The doctor, often a primary care physician (general practitioner, GP) initially, will carry out a physical exam, and then refer the patient to a specialist if he/she thinks further assessment is needed.
Below are examples of diagnostic tests and procedures for breast cancer:
- Breast exam – the physician will check both the patient’s breasts, looking out for lumps and other possible abnormalities, such as inverted nipples, nipple discharge, or change in breast shape. The patient will be asked to sit/stand with her arms in different positions, such as above her head and by her sides.
- X-ray (mammogram) – commonly used for breast cancer screening. If anything unusual is found, the doctor may order a diagnostic mammogram.
- 2D combined with 3D mammograms – 3D mammograms, when used in collaboration with regular 2D mammograms were found to reduce the incidence of false positives.
- Breast ultrasound – this type of scan may help doctors decide whether a lump or abnormality is a solid mass or a fluid-filled cyst.
- Biopsy – a sample of tissue from an apparent abnormality, such as a lump, is surgically removed and sent to the lab for analysis. If the cells are found to be cancerous, the lab will also determine what type of breast cancer it is, and the grade of cancer (aggressiveness).
- Breast MRI (magnetic resonance imaging) scan – a dye is injected into the patient. This type of scan helps the doctor determine the extent of the cancer.
- Staging describes the extent of the cancer in the patient’s body and is based on whether it is invasive or non-invasive, how large the tumor is, whether lymph nodes are involved and how many, and whether it has metastasized (spread to other parts of the body).A cancer’s stage is a crucial factor in deciding what treatment options to recommend, and in determining the patient’s prognosis.
Staging is done after cancer is diagnosed. To do the staging, the doctor may order several different tests, including blood tests, a mammogram, a chest X-ray, a bone scan, a CT scan, or a
PET scan.
Treatment.
Treatment for breast cancer, which includes surgery, radiation and chemotherapy, causes many patients to experience pain and stiffness in the chest, shoulder and back muscles, as well as initial swelling and numbness near a surgical incision site. Other common side effects of breast cancer treatment include nerve irritation, as radiation and surgery can cause nerves to become swollen, which can result in numbness, pain or tingling sensations. Fatigue is also common and can easily overwhelm a patient.
An integrated, multidisciplinary team of physicians, nurses, physical therapists, occupational therapist and social workers can help identify a patient’s rehabilitation needs.
Breast Cancer Rehabilitation
Breast cancer rehabilitation provides treatment for many common physical difficulties experienced by breast cancer patients and survivors. If you answer “yes” to any of the following questions, our breast cancer rehabilitation services may be able to help:
- Do you have pain in your chest or shoulder area?
- Do you feel stiff or tight in your chest or shoulder area?
- Is it hard to bathe, dress or do your household chores because of pain and difficulty moving your arm?
- Does your arm feel heavy or tired?
- Are you feeling overwhelmingly fatigued?
- Do you feel weak?
If you are experiencing any of the issues noted above, please speak to your physician about breast cancer rehabilitation treatment; a physician’s prescription/order is required for these services.
Breast Cancer Rehabilitation Treatment
Rehabilitation services may include:
- Exercises to
- Improve range of motion
- Improve strength
- Improve posture
- Reduce pain
- Hands-on treatment to improve soft-tissue mobility
- Education to help you learn
- Which exercises and activities can be done at home
- How to reduce your risk of lymphedema
- Lymphedema screening and treatment
Breast Cancer Rehabilitation Can Be Performed
- After surgery or biopsy
- During or after chemotherapy or radiation treatment
- Before, during or after breast reconstruction
- Years after breast cancer care
Rehab Experts offers a variety of in-patient and out-patient services to alleviate the physical impact of surgery and medical management following breast cancer diagnosis. Our therapists work closely with surgeons, medical oncologists and radiation oncologists to provide physical therapy services to patients throughout the continuum of care for breast cancer.
Our physical therapists working with individuals with breast cancer are experts in the field who are dedicated to ensuring patients achieve the highest level of function and quality of life following cancer treatment.
physical therapy home service
Visit Our Google + Page
References:
Medical News Today. http://www.medicalnewstoday.com/articles/37136.php
Beth Israel Deaconess Medical Center http://www.bidmc.org/YourHealth/HealthNotes/BreastHealth/LatestNews/PhysicalTherapy.aspx