A stroke, or cerebrovascular accident (CVA), is an infarction of the brain in which ischemia or hemorrhage causes disruption of function. Characterized by sudden onser focal neurological deficit, hemiparesis is the hallmark of stroke. The logical deficit, hemiparesis is the hallmark of stroke. The terms CVA and stroke are generally used interchangeable. To avoid confusion, use a description such as right CVA with left hemiparesis.
Etiology/Pathophysiology
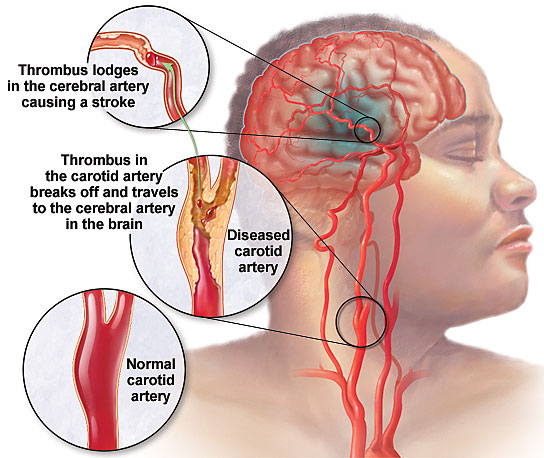
There are four major forms of vascular disease of the brain. Thrombotic strokes are usually due to atherosclerotic stenosis or occlusion of the carotid or middle cerebral artery. The deficit may be preceded by transient ischemic attacks (TIAs) or evolve over time, since thrombotic occlusion occurs gradually. Embolic strokes, in contrast, occur abruptly as platelets, cholesterol, fibrin, or other blood components float in the circulation until they occlude small distal cortical vessels. Strokes occurring in the setting of myocardial infarction are usually a result of cardiac emboli. Lacunar strokes are very small infarction, less than 1cm3, occurring where small perforating arterioles branch directly off large vessels. Hemorrhagic stroke is the most catastrophic. Regions of the brain affected are similar to those affected in lacunar stroke, including the basal ganglia, internal capsule, and brainstem.
Assessment/Evaluation
Perform a thorough neurological evaluation, including history and physical examination at the time of presentation. Repeat it frequently to asses further neurologic deficit. Document risk factors. Routine diagnostic evaluations may include computerized axial tomography (CAT scan) of the head, electroencephalogram (EEG), magnetic resonance imaging (MRI), carotid Doppler studies, cardiac evaluation, including 2-D echocardiograms as well as electrocardiogram (EKG), and routine bloodwork with clotting times. These studies are undertaken to determine cause of the stroke, so that risk factors may be addressed.
Typical patterns of deficits occur that may aid in localization of ischemic stroke. Lesions of the anterior cerebral artery usually result in paralysis and cortical hypesthesia of the contralateral lower limb, with mild involvement of the contralateral arm. There may be impaired judgement and insight, incontinence of bowel and bladder, apraxia of gait, and sucking and grasping reflexes of the contralateral side.
Middle, cerebral infarction typically produces contralateral hemigplegia. Usually, the arm is more affected than the leg. Sensation is impaired in the same areas as motor loss (cortical sensory deficit, or cortical hypesthesia). Blindness in one half of the visual field (hemianopsia), inability to recognize persons and things (agnosia), or difficulty in communicating (dysphasia) may occur.
Brain stem strokes either leave minor deficits, or are so severe that recovery is rare. Typical brain stem deficits include swallowing, visual, and balance problems.
Functional Evaluation
Several functional evaluation scales have been devised for use in stroke and other disabilities. The most widely accepted is the Functional Independence Measure (FIM). The FIM involves seven levels of function within six areas, including self-care, sphincter management, mobility, locomotion, communication, and social cognition.
Treatment
Traditional stroke rehabilitation employs the use of compensatory techniques for mobility, activities of daily living (ADLs), and communication while natural recovery, to the extent possible, occurs over time. A limited time trial of inpatient rehabilitation (2 weeks or less) allows a patient to demonstrate his appropriateness ass a candidate for further inpatient rehabilitation immediately following acute stroke. Poor prognostic indicators for stroke rehabilitation candidates.
Stokes are common events, yet stroke rehabilitation is complex. Even though functional deficits appear to be similar, patients react individually. Therefore, each stroke rehabilitation program must be uniquely tailored. Even more important than physical deficits are the cognitive aspects affected by stroke. The left-brain injured, functionally right hemiplegic patient is much different with respect to communication and learning than the right-brain injured, functionally-left hemiplegic patient. These differences must be recognized and addressed in treatment.
Rehabilitation of the stroke patient begins in the acute care setting. Timely intervention maximizes potential recovery and prevents problems due to immobility.
Medical treatment of stroke consists of evaluation of the cause of the stroke and correction of underlying problems, if possible. One aspirin a day is the current accepted treatment for the patient who has sustained a thrombotic stroke. Dipyridamole (Persantine) has not been shown to be efficacious. Ticlopidine (Ticlid),250 mg orally twice daily, is indicated in thrombotic stroke if aspirin is not tolerated. Embolic stroke patients should undergo thorough cardiovascular examinations, and be anticoagulated, long-term, if indicated. Lacunar and hemorrhagic stroke patients with elevated blood pressures may require antihypertensive medications.
There is little surgical intervention for acute stroke. Ipsilateral carotid endarterectomy is indicated for patients who have TIAs or mild or recovered strokes, who have angiography-documented carotid stenosis of 70% or more.
[tagline_box link=”http://www.rehabexperts.com.ph/contact-us” linktarget=”” button=”Contact us now!” title=”Physical Therapy Home Service” description=”Are you a person suffering from some physical disabilities? Do you intend to find a solution to your physical disabilities? Are you already tired masking the pain and intend to find a solution to your physical disabilities? Do you intend to address the root-cause of pain and find a lasting remedy to your physical disabilities? Are you looking for a good quality physical therapy home service?”][/tagline_box]
Resources:


